Health Library
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Coronary Artery Disease
Condition Basics
What is coronary artery disease?
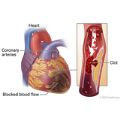
Coronary artery disease, or heart disease, is a heart problem that happens when fatty deposits called plaque (say "plak") build up inside coronary arteries of your heart. Those are the blood vessels that supply blood and oxygen to your heart muscle. This process of plaque buildup is called hardening of the arteries, or atherosclerosis.
Plaque buildup may reduce blood flow to the heart muscle. Like any muscle, the heart needs blood to work well. Poor blood flow can cause angina symptoms, such as chest pain or pressure. If the plaque breaks apart, it can cause a heart attack.
What causes it?
Coronary artery disease is caused by a process called hardening of the arteries, or atherosclerosis. Fatty deposits called plaque build up inside coronary arteries. These arteries supply blood to the heart muscle. Over time, the plaque buildup may narrow the arteries and reduce blood flow to the heart muscle.
What are the symptoms?
The symptoms of coronary artery disease are angina and shortness of breath. Angina can feel like chest pain or pressure. Some people feel pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or in one or both shoulders or arms. Symptoms typically happen when the heart works hard.
How is it diagnosed?
Your doctor will ask about your medical history and do a physical exam. You may have tests to check how well your heart is working and to see if your arteries are narrowed. Examples of tests include an electrocardiogram, an echocardiogram, stress tests, and a CT angiogram.
How is coronary artery disease treated?
Coronary artery disease is treated with healthy lifestyle changes and medicine. Treatment focuses on lowering your risk for heart attack and stroke and managing your symptoms. Sometimes angioplasty or bypass surgery is done to improve blood flow to the heart.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Aspirin: Should I Take Daily Aspirin to Prevent a Heart Attack or Stroke?
- Coronary Artery Disease: Should I Have an Angiogram?
- Coronary Artery Disease: Should I Have Angioplasty for Stable Angina?
- Coronary Artery Disease: Should I Have Bypass Surgery?
- High Blood Pressure: Should I Take Medicine?
- Statins: Should I Take Them to Prevent a Heart Attack or Stroke?
Cause
Coronary artery disease is caused by a process called hardening of the arteries, or atherosclerosis.
Atherosclerosis occurs when fatty deposits called plaque build up inside arteries. Arteries are the blood vessels that carry oxygen-rich blood throughout your body. When plaque builds up in the arteries that supply blood to the heart muscle (the coronary arteries), it is called coronary artery disease. Over time, the plaque may narrow the arteries and reduce blood flow to the heart muscle.
Learn more
What Increases Your Risk
Things that put you at risk for coronary artery disease are the things that lead to a problem called atherosclerosis, or hardening of the arteries. These things include:
- High cholesterol.
- High blood pressure.
- Diabetes.
- Smoking.
- Being overweight.
- A family history of early heart disease. Early heart disease means you have a male family member who was diagnosed before age 55 or a female family member who was diagnosed before age 65.
Your age, sex, and race can also raise your risk. For example, your risk increases as you get older.
Learn more
Prevention
You can help prevent coronary artery disease by taking steps toward a heart-healthy lifestyle. A heart-healthy lifestyle can also help you reduce risk factors such as high cholesterol and high blood pressure.
- Quit smoking, and avoid secondhand smoke.
This is one of the best things you can do for your heart and your overall health.
- Be active.
- Try to do moderate activity at least 2½ hours a week. Or try to do vigorous activity at least 1¼ hours a week. Physical activity, like walking, can help you lose weight, lower your blood pressure, and improve your cholesterol.
- Before you start an activity, talk to your doctor to find out how much is safe for you. Increase your activity a little bit at a time, as your doctor approves.
- Eat heart-healthy foods.
This means eating plenty of fruits and vegetables, fish, and high-fiber grains and breads. Eat foods low in sodium (salt), saturated fat, and trans fat. Limit alcohol and sugar.
- Stay at a healthy weight.
Being overweight makes you more likely to have high blood pressure, heart problems, and diabetes. These conditions make a heart attack more likely.
- Manage other health problems.
Health problems such as diabetes, high blood pressure, and high cholesterol can make having heart problems more likely. If you manage these conditions, you can lower your risk for heart problems. Lifestyle changes can help you manage these other health problems.
If you think you may have a problem with alcohol or drug use, talk to your doctor.
Learn more
Symptoms
The symptoms of coronary artery disease are angina (say "ANN-juh-nuh" or "ann-JY-nuh") and shortness of breath. Symptoms can happen when the heart is working hard and does not get enough oxygen, such as during exercise. Some people don't have any symptoms.
Angina
People feel angina symptoms in different ways. Symptoms include chest pain or pressure, or a strange feeling in the chest. Some people feel pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or in one or both shoulders or arms. Other symptoms of angina include shortness of breath, nausea or vomiting, lightheadedness or sudden weakness, and a fast or irregular heartbeat.
Some people describe their angina as pressure, heaviness, weight, tightness, squeezing, discomfort, or dull aching in the chest. People may put a fist to the chest when describing their pain. Some people may feel tingling or numbness in the arm, hand, or jaw.
Most people feel angina symptoms in the chest. Women are somewhat more likely than men to have other symptoms like shortness of breath, nausea, and back or jaw pain. Some women describe their symptoms as mild. Others feel tired when they have angina.
Angina can be stable or unstable.
- Stable angina means that you can usually predict when your symptoms will happen. You probably know what things cause your angina. For example, you know how much activity usually causes your angina. You also know how to relieve your symptoms with rest or nitroglycerin.
- Unstable angina means that your symptoms have changed from your typical pattern of stable angina. Your symptoms do not happen at a predictable time. For example, you may feel angina when you are resting. Your symptoms may not go away with rest or nitroglycerin.
Silent ischemia
Some people don't have any symptoms. This is called "silent ischemia." Ischemia is the medical term for what happens when your heart muscle doesn't get enough oxygen.
Heart attack
A heart attack is sometimes the first sign of coronary artery disease.
What Happens
Coronary artery disease is a lifelong (chronic) disease. It can get worse over time and can lead to a heart attack or other heart problems. But treatment can help slow the disease, relieve symptoms, and prevent a heart attack.
Atherosclerosis (hardening of the arteries)
Coronary artery disease most often begins when the inside walls of the coronary arteries are damaged because of another health problem, such as high cholesterol, high blood pressure, diabetes, or smoking. This damage can lead to atherosclerosis, or hardening of the arteries. This means that plaque, made of fats and other substances, builds up in the coronary arteries.
Atherosclerosis can get worse over time. As plaque builds up in the arteries, they may become narrow. This can reduce blood flow to the heart muscle. This is called ischemia (say "is-KEE-mee-uh"). Ischemia can cause angina symptoms, such as chest pain or pressure.
Angina symptoms
Some people with coronary artery disease never feel angina symptoms, such as chest pain or pressure. But others may feel angina symptoms when their hearts have to work harder, such as during exercise. Angina is a signal that your heart is not getting enough oxygen.
If you've had angina for a while, you may be able to predict what activities or stress will cause your symptoms. This is called stable angina.
If coronary artery disease gets worse, your stable angina symptoms may change. For example, you can still predict when symptoms will happen, but they may come on sooner, feel worse, or last longer.
If blood flow to the heart muscle is suddenly slowed, unstable angina happens. Unstable angina is an emergency. It may mean that you are having a heart attack.
Unstable angina is a change in your usual pattern of stable angina. Your symptoms do not happen at a predictable time. For example, you may feel angina when you are resting. Your symptoms may be more frequent, severe, or longer-lasting than your usual pattern of stable angina. Your symptoms may not go away when you try your typical ways of relieving them, such as rest or nitroglycerin.
Heart attack
If the plaque in a coronary artery breaks apart, it can cause a heart attack. A tear or rupture in the plaque tells the body to repair the injured artery lining, much as the body might heal a cut on the skin. A blood clot forms to seal the area. The blood clot can completely block blood flow to the heart muscle and cause a heart attack.
Other heart problems
Over time, low blood flow to the heart muscle can weaken or damage the heart. This can lead to heart failure or atrial fibrillation.
Heart attacks that damage critical or large areas of the heart tend to cause more problems (complications) later. These may include:
- Arrhythmias (heart rhythm problems).
- Heart failure.
- Heart valve disease.
Learn more
When to Call a Doctor
Do not wait if you think you are having a heart attack. Some people aren't sure whether they're having one, or they don't want to bother others, so they wait. But getting help fast can save your life.
Call 911 or other emergency services immediately if you have symptoms of a heart attack or are with someone who has symptoms. Symptoms may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
After you call 911, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself. By taking an ambulance, you may be able to start treatment before you arrive at the hospital.
Nitroglycerin. If you typically use nitroglycerin to relieve angina and if one dose of nitroglycerin has not relieved your symptoms within 5 minutes, call 911. Do not wait to call for help.
Call your doctor if:
- Your angina symptoms are different, more frequent, or severe.
Exams and Tests
Your doctor will do a physical exam, a medical history, and possibly some tests to find out if you have coronary artery disease or are at risk for having it.
Medical history and physical exam
A medical history and physical exam are always a part of evaluating a person who has symptoms or risk factors for coronary artery disease. The history and physical exam help to guide further decisions about testing and treatment.
During the medical history, your doctor will ask questions about your symptoms, your personal health history, and your family medical history.
A complete physical exam will also be done. This includes checking your blood pressure and listening to your heart and lungs.
Tests
If your doctor thinks you may have coronary artery disease, you will have some tests. They include:
- An electrocardiogram (EKG or ECG) to measure the electrical signals that control the heartbeat.
- A chest X-ray to see your heart, lungs, and major blood vessels.
- An exercise electrocardiogram to check for changes in your heart while you exercise. This is also called a "stress test."
You might have one or more imaging tests to look at your arteries and your heart. You might have these tests if your doctor needs more information for diagnosis or to help guide treatment.
These tests include:
- Stress echocardiogram, cardiac perfusion scan, or other types of stress tests. These tests look at blood flow to the heart muscle and how well the heart is working.
- CT angiogram to check blood flow in the coronary arteries.
- Coronary angiogram. This is an invasive test to look at blood flow in the coronary arteries.
Learn more
Treatment Overview
Coronary artery disease is treated with healthy lifestyle changes and medicine. Sometimes a procedure or surgery is done.
Treatment focuses on lowering your risk for heart attack and stroke and managing your symptoms. It can slow the disease and improve the quality and length of your life.
- Lifestyle changes include being active, not smoking, eating heart-healthy foods, staying at a healthy weight, and managing other health problems. A cardiac rehab program can help you make these changes.
- Medicines can help you lower cholesterol and high blood pressure, manage angina, and lower your risk of having a blood clot.
- Procedures that improve blood flow to the heart include angioplasty and bypass surgery. These might be done to relieve angina. Or they might be done to treat a heart attack.
Learn more
Self-Care
There are many things you can do to feel better, prevent problems, and stay healthy longer. These steps are an important part of treatment.
You can lower your risk for heart attack and stroke by making lifestyle changes and taking medicine. A heart-healthy lifestyle can also improve the quality and length of your life.
Take medicine properly
Taking medicine correctly can lower your risk of having a heart attack or dying from coronary artery disease.
- Take your medicines exactly as directed. You may take several medicines.
- Do not stop taking your medicine unless your doctor tells you to.
- Talk with your doctor before you take any over-the-counter medicines, vitamins, or herbal products. If you need to take an NSAID for a long time, talk with your doctor to see if it is safe for you.
Have a heart-healthy lifestyle
Lifestyle changes are the first step for anyone with coronary artery disease. Even though you take medicine, lifestyle changes can also keep your heart and your body healthy.
Healthy habits can slow the disease. They can improve the quality and length of your life. And they can help lower your risk of a heart attack and stroke.
Ask your doctor if a cardiac rehabilitation (rehab) program is right for you. In cardiac rehab, you will get support to help you build new, healthy habits.
To be heart-healthy:
- Don't smoke. Avoid secondhand smoke.
- Quitting smoking is the best thing you can do to reduce your risk of future problems. When you quit, you lower your risk of a heart attack.
- Be active.
- Being active can help your heart get stronger and work better. Talk to your doctor before you start an exercise program. Make sure that it's safe for you.
- Eat a heart-healthy diet.
- Healthy foods can help you stay at a healthy weight and manage other health problems such as high blood pressure and diabetes.
- Stay at a healthy weight.
- Lose weight if you need to. A healthy weight can help keep your heart and body as healthy as possible.
Manage angina symptoms
- Pay attention to your symptoms.
- Then you can see what causes them and what is typical for you.
- Know how to manage angina.
- Most people can control their symptoms by taking medicine or changing their activities.
- Know when to call your doctor or get help right away.
Call your doctor if your stable angina symptoms seem worse but still follow your typical pattern. You can predict when symptoms will happen, but they may come on sooner, feel worse, or last longer.
Get help right away if you have angina symptoms that do not follow your typical pattern. For example, your symptoms may happen at rest or not go away with nitroglycerin. It may mean you are having a heart attack.
Manage and prevent other health problems
- Manage other health problems that raise your risk for a heart attack or stroke.
- These include diabetes, high blood pressure, and high cholesterol.
- Avoid infections such as COVID-19, colds, and the flu.
- Get the flu vaccine every year. Get a pneumococcal vaccine. If you have had one before, ask your doctor whether you need another dose. Stay up to date on your COVID-19 vaccines.
- Get help for depression.
- Depression is a medical problem that needs treatment. Getting treatment can help you stay healthy.
- Talk with your doctor if you think you have a problem with alcohol or drug use.
- This includes prescription medicines (such as amphetamines and opioids) and illegal drugs (such as cocaine and methamphetamine).
Take other steps to stay healthy
- Manage stress.
- Stress can be bad for your heart and might make your symptoms worse.
- Drink alcohol in moderation, if you drink.
- This means having no more than 1 drink a day for women or 2 drinks a day for men.
- Seek help for sleep problems.
- Sleep apnea is a common problem in people who have heart disease.
- Find emotional support.
- Support from friends and family is important whether you are recovering from a heart attack or are changing your lifestyle so you can avoid one.
- Have sex when you're ready.
- Sex is part of a healthy life. And it can be safe for people who have heart problems. Your doctor can help you know if your heart is healthy enough for sex.
Learn more
- Coronary Artery Disease: Exercising for a Healthy Heart
- Coronary Artery Disease: Helping a Loved One
- Depression and Anxiety When You Have Coronary Artery Disease
- Heart-Healthy Eating
- Manage Stress for Your Heart
- Quick Tips: Taking Charge of Your Angina
- Quitting Smoking
- Sex and Your Heart
- Weight Management
Medicines
Medicines are an important part of your treatment for coronary artery disease. A few medicines work in different ways to help lower your risk of having a heart attack or dying from coronary artery disease. These medicines help lower blood pressure, lower cholesterol, lower the heart's workload, and prevent blood clots.
Medicines are also used to help relieve your symptoms.
Medicine that lowers blood pressure and the heart's workload
These medicines include:
- Angiotensin-converting enzyme (ACE) inhibitors.
- Angiotensin II receptor blockers (ARBs).
- Beta-blockers.
- Calcium channel blockers.
- Diuretics.
Medicine that prevents blood clots
Aspirin and other blood thinners can help prevent blood clots from forming that could cause a heart attack.
Aspirin, ibuprofen, and naproxen are all nonsteroidal anti-inflammatory drugs (NSAIDs). They can relieve pain and inflammation. But only aspirin will reduce your risk for heart attack or stroke. Don't substitute ibuprofen or naproxen for aspirin.
Medicine that lowers cholesterol
Statins help lower cholesterol. Other cholesterol medicines, such as ezetimibe, may be used along with a statin.
Medicine that relieves angina symptoms
Stable angina can often be controlled with medicine such as:
- Nitrates (nitroglycerin and long-acting nitrates).
- Beta-blockers.
- Calcium channel blockers.
- Ranolazine (Ranexa).
Learn more
- Angiotensin-Converting Enzyme (ACE) Inhibitors
- Angiotensin II Receptor Blockers (ARBs)
- Anticoagulants
- Antiplatelets
- Aspirin: Should I Take Daily Aspirin to Prevent a Heart Attack or Stroke?
- Beta-Blockers
- Blood Thinners Other Than Warfarin: Taking Them Safely
- High Blood Pressure: Should I Take Medicine?
- Statins
- Statins: Should I Take Them to Prevent a Heart Attack or Stroke?
- Using Nitroglycerin for Angina
Procedures That Improve Blood Flow
Coronary artery bypass surgery
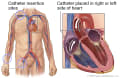
Coronary artery bypass surgery is a surgery to treat coronary artery disease. The surgery helps blood make a detour, or bypass, around one or more narrowed or blocked coronary arteries. Coronary arteries are the blood vessels that bring blood to the heart. The surgery is also called bypass surgery or coronary artery bypass graft (CABG).
Your doctor will make a bypass using a piece of blood vessel from another part of your body. Your doctor will attach, or graft, this blood vessel above and below the narrowed or blocked section of your artery.
Angioplasty
Coronary angioplasty is a procedure that uses a thin tube called a catheter to open a blocked or narrowed coronary artery. Coronary arteries are the blood vessels that bring oxygen to the heart muscle. Angioplasty also may be called percutaneous coronary intervention (PCI).
Angioplasty can widen an artery that has been narrowed by fatty buildup (plaque) or blocked by a blood clot. The procedure helps blood flow more normally to the heart muscle.
Learn more
Related Information
Credits
Current as of: October 2, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 2, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.